Many of the symptoms of hypothyroidism are similar to the symptoms of vitamin B12 deficiency. Thus, fatigue, weakness, depression, irritability, memory loss, abnormal menstrual cycles, decreased libido and poor mental growth are similar. to both conditions. Confounding the situation is that there is a high (approx 40%) prevalence of vitamin B12 deficiency in hypothyroid patients (Jabbar etal, 2008). Traditional symptoms are not a good guide to determining presence of B12 deficiency. Screening for vitamin B12 levels should be undertaken in all hypothyroid patients, irrespective of their thyroid antibody status.
Normal cycling of folate results in the formation of an irreversible reaction in which 5, 10 methylenetetrahydrofolate is converted to 5-methyltetrahydrydrofolate (5-MTHF) by the enzyme 5,10 methyltetrahydrofolate reductase (MTHFR). Of note in this reaction is that MTHFR uses FAD (derived from riboflavin, vitamin B2) as an essential cofactor. In addition, the reduction that occurs requires input from NADH + H+ (derived from nicotinamide, vitamin B3). In the absence of these two vitamins (B2/B3) the enzyme is not functional. In this situation, folate is not able to recycle via the conversion of 5,10-methenyltetrahydrofolate to 5-methyltetrahydrofolate. This leads to an intracellular deficiency of folate, MeCbl, methionine and SAM. Furthermore, the regeneration of reduced *Co(I)VB12) that often becomes oxidized to inactive Co(II)VB12 requires the FMN/FAD dependent methionine synthase reductase (MTRR), and lack of FAD due to hypothyroidism decreases the activity of this enzyme and hence VB12 used by methionine synthase cannot be recycled.
In addition, often in hypothyroidism there is inefficient stimulation of gastric acid production and release of intrinsic factor from the parietal cells in the intestine. This lack of gastric acid reduces the activity of pepsin in the stomach leading to incomplete digestion/extraction of vitamin B12, iron and riboflavin from food. This in itself can lead to vitamin B12 deficiency.
Folate Cycle
FAD, P5P in production of 5MTHF
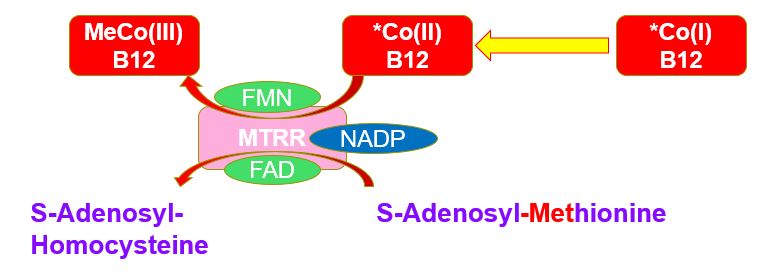
FMN/FAD in regeneration of MethyCo(III)B12
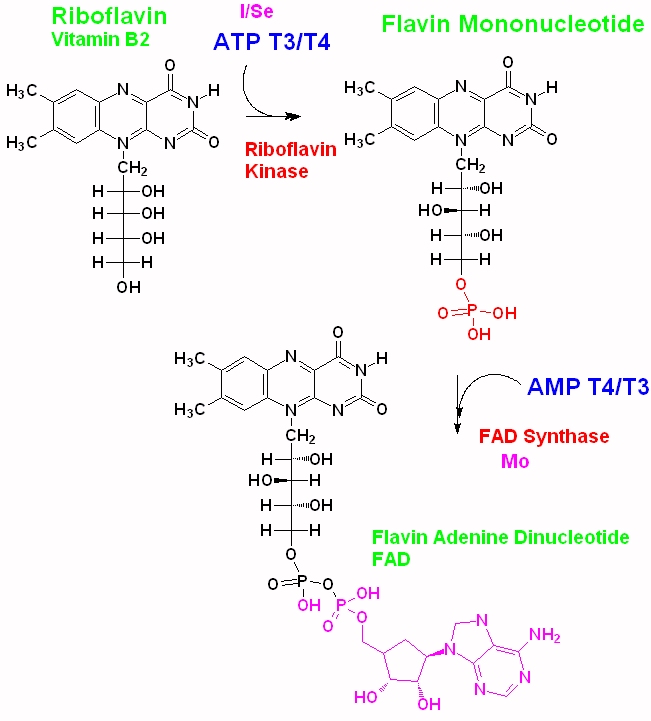
Synthesis of Flavin Mononucleotide (FMN) from riboflavin requires the addition of phosphate from ATP, via riboflavin kinase, with the input of triiodothryonine (T3) and thyroxine (T4). Both T3 and T4 are produced in the thyroid following stimulation by thyroid stimulating hormone (TSH). The subsequent synthesis of FAD from FMN also involves contribution of thyroxin in the presence of FAD plus AMP. Deficiency in thyroxine, due to hypothyroidism can result in reduced levels of FAD in the body. Similarly dietary deficiency in either iodine (required for synthesis of T4), selenium (required for the conversion of T4 to T3), molybdenum (for the conversion of FMN to FAD) and/or riboflavin can result in reduced FAD, subsequently resulting in vitamin B12 deficiency.
In persons consuming sufficient dietary vitamin B12, the gradual inactivation of vitamin B12 due to the deficiency in FMN and FAD, generally will lead to an accumulation of inactive vitamin B12 in serum, and will not result in lowering of serum vitamin B12, and may result in a gradual increase in circulating levels of vitamin B12.. In this case, the hypothyroidic individual may show many of the signs of vitamin B12 deficiency, but the deficiency will be missed unless functional tests of vitamin B12 activity are performed. As such the person will have "Paradoxical vitamin B12" deficiency, in which serum B12 levels are "normal" or elevated, yet the person has many or the classical signs of vitamin B12 deficiency, such as constant lack of energy, an inability to concentrate, depression, anxiety, constant mood swings, a lack of motivation, and difficulty sleeping, amongst others. Other markers that may be raised are homocysteine and MMA.(Jabbar etal, 2008; Zaric etal, 2019).
Several studies on vitamin B12 supplementation have used either cyanocoblamin (CN-B12) or hydroxylcobalamin (OH-B12) and up to 50% of the patients were found not to respond to the B12 supplements either in reduction of symptoms or in the lowering of homocysteine and/or MMA. Whilst FAD levels were not tested in these individuals, low FAD (from vitamin B2, or hypothyroidism) would lead to an inability to reduce OH-B12 or CN-B12 to adenosyl and/or methyl B12.
From the above it is obvious that a single nutrient deficiency in any of Iodine, Selenium, Molybdenum and vitamin B2, can or will lead to lack of functional B2, and this will eventually lead to inactivation of vitamin B12, and result in functional B12 deficiency. This deficiency, though may not and generally does not result in lowering of vitamin B12, in fact the opposite can occur, in that the is a gradual accumulation of more and more inactive B12 in serum, leading to a condition of Paradoxical B12 deficiency, in which serum B12 is higher than normal, yet the individual accumulates more and more symptoms of vitamin B12 deficiency. In this case, vitamin B12 supplementation is generally ineffective, particularly via the oral route, unless the functional B2 deficiency is resolved (Russell-Jones, 2022).
In order for vitamin B12 supplementation to be optimally effective in persons who have hypothyroidism, functional vitamin B2 deficiency, which has resulted from the hypothyroidism must be treated first. Effective treatment can often be achieved by ensuring that the person has sufficient Iodine (150-300 ug/day) and Selenium (as Selenite, or Selenate)(55-200 ug/day), and Molybdenum (as Molybdate)(100-300 ug/day)..
Jabbar etal, Vitamin B12 deficiency common in primary hypothyroidism. J Pak Med Assoc. 2008 May;58(5):258-61
Zaric etal, Homocysteine and hyperhomocysteinaemia. Curr Med Chem 2019;26(16):2948-2961
Russell-Jones, G.J 2022 Paradoxical B12 deficiency: Normal to elevated serum vitamin B12 with metabolic vitamin B12 deficiency. PDF https://www.iomcworld.org/articles/paradoxical-vitamin-b12-deficiency-normal-to-elevated-serum-b12-with-metabolic-vitamin-b12-deficiency.pdf
Copyright © 2018
vitaminb12deficiency.info. All Rights Reserved.
The statements on this site compose a compendium of generally recognized signs
of vitamin B12 deficiency, and problems that can then ensue They also are formulated from a summary of relevant
scientific publications. In addition they may contain some forward looking
statements of a general nature.
Reproduction in whole or in part in any form or medium without express written
permission is prohibited